ISFGS App
The Fluorescence-Guided Surgery App provides surgeons and trainees with instant access to expert content and practical guidance on fluorescence imaging — anytime, anywhere.
We are dedicated to the global advancement of fluorescence image-guided surgery through clinical practice, education, and the promotion of basic and clinical research.
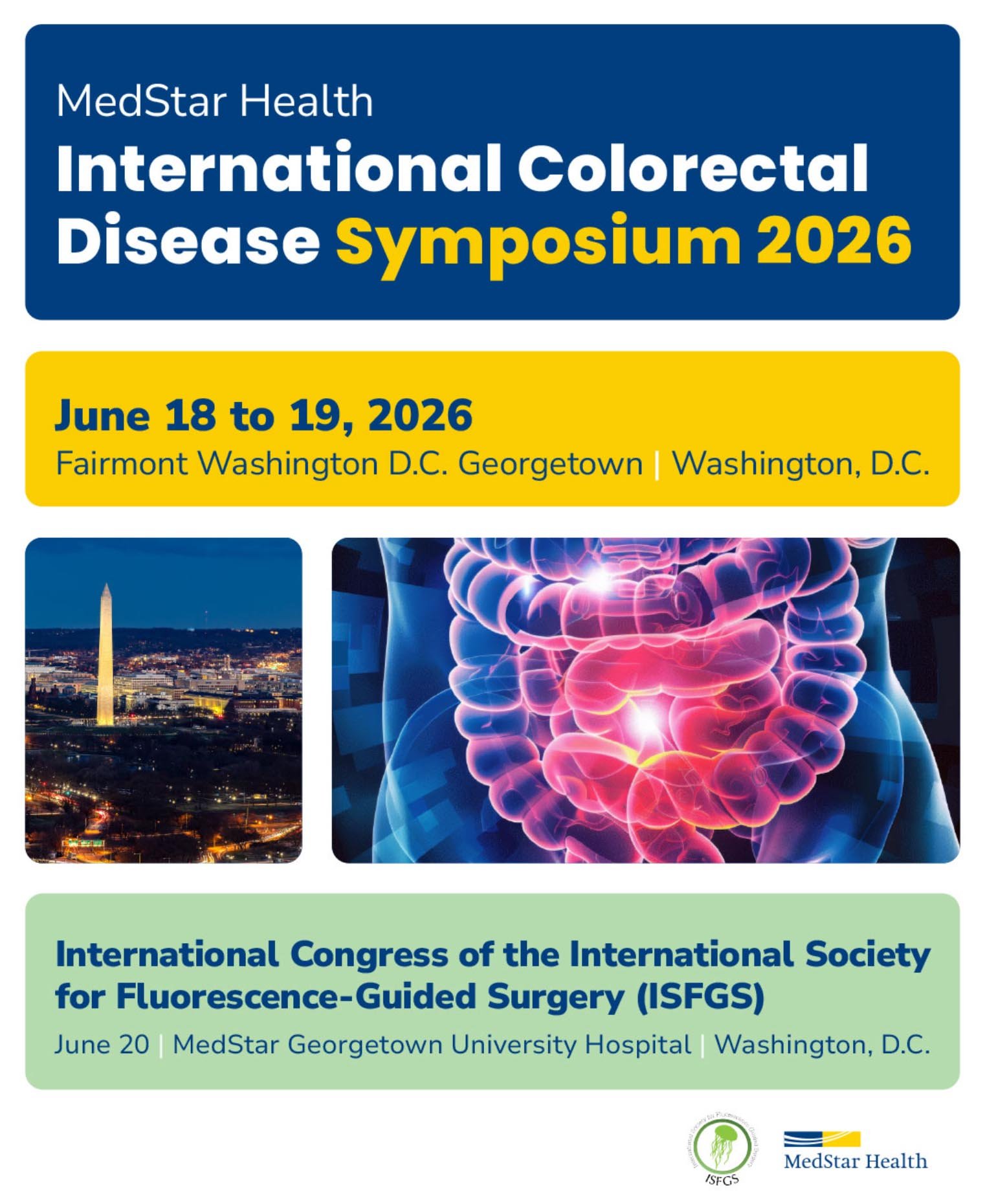
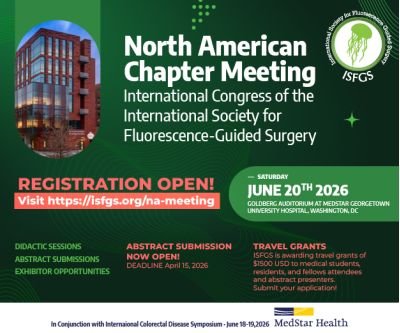
Upcoming events
Stay updated, sign up for our Newsletter
We are building this website together. Do you have content to share? Send it to us at This email address is being protected from spambots. You need JavaScript enabled to view it.
We are building this website together. Do you have content to share? Send it to us at This email address is being protected from spambots. You need JavaScript enabled to view it.